50F with pyrexia under evaluation
50 year old female, health care worker ( aayamma in orthopedic hospital ) resident of miryalguda presented with complaints of fever since 1 week, nausea and vomitings for 3 days, Rt shoulder pain since 1 week.
C/O FEVER SINCE 1 WEEK ASSOCIATED WITH VOMITINGS
HOPI:
PATIENT WAS APPARENTLY ASYMPTOMATIC 30 DAYS BACK THEN SHE DEVELOPED FEVER OF HIGH GRADE WITH CHILLS AND RIGORS FOR WHICH SHE GOT ADMITTED IN HOSPITAL AND TREATED , FEVER RELIVED ON MEDICATION.
SINCE 1 WEEK SHE DEVELOPED FEVER OF HIGH GRADE WITH CHILLS AND RIGORS, CONTINUOUS RELIEVED ON MEDICATION BUT RECURRING AFTER 3-4 HRS, GENERALISED WEAKNESS PRESENT, DRY MOUTH PRESENT, VOMITINGS PRESENT 2-3 EPISODES PER DAY SINCE 1 WEEK , NON BILIOUS, PROJECTILE, CONTAIN FOOD PARTICLES, 1 EPISODE OF BILIOUS VOMITING TODAY MORNING, NAUSEA PRESENT, LOSS OF APETITE PRESENT.
NO H/O LOSS OF WEIGHT, SORE THROAT, COUGH, COLD, ABDOMINAL PAIN , DIARRHEA, BURNING MICTURITION.
PAST HISTORY:
N/K/C/O DM, HTN, THYROID, ASTHMA, CAD, CVA, EPILEPSY
FAMILY HISTORY : INSIGNIFICANT
GENERAL EXAMINATION:
PATIENT IS C/C/C
NOPALLOR,ICTERUS,CYANOSIS,CLUBBING,LYMPHADENOPATHY,ODEMA.
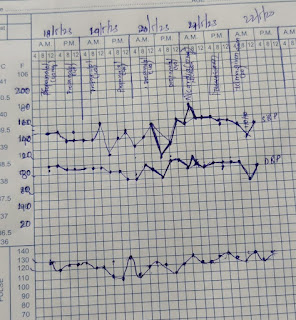
VITALS: TEMP: 100.8 F
PR:134 BPM
BP:130/80
RR:20 CPM
SPOI2: 98%
GRBS:102 MG%
SYSTEMIC EXAMINATION:
CVS:S1,S2 +
CNS:NAD,
RS:BAE+, NAD.
PA:SOFT,NONTENDER, NO ORGANOMEGALY
CARDIOLOGY REFFERAL DONE ON 12/5/23 I/V/O PERSISTENT TACHYCARDIA (MORE THAN 110-120 BPM) ,AND ADVISED TAB.MET-XL 25 MG PO/OD.
ORTHOPAEDICS REFFERAL DONE ON 12/5/23 I/V/O B/L KNEE JOINT PAIN AND RIGHT SHOULDER PAIN ,AND ADVISEDTAB.FEBUXOSTAT 40MG PO/OD (
ENT REFERRAL DONE ON 13/5/23 DIAGNOSED AS LARYNGOPHARYNGOREFLUX DISEASE ADVISED USG NECK AND UPPER GI ENDOSCOPY TREATED WITH CANDID ORAL PAINT,ZYTEE,SYP.SUCRAFYL
PSYCHIATRY REFERRAL DONE ON 21/5/23 I/V/O DELIRIUM ADVISED
SURGERY REFERRAL DONE ON 22/5/23 I/V/O NECK SWELLING WHICH ON ULTRASOUND SHOWED DIFFUSE THYROPIDITIS TIRADS 3 LESION IN LEFT LOBE OF THYROID DIAGNOSE AS DIFFUSE GOITRE AND ADVISED FNAC
INVESTIGATIONS :
2D ECHO
USG NECLK- DIFFUSE THYROIDITIS, TIRADS 3 LESION IN LEFT LOBER OF THYROID
USG RIGHT SHOULDER _BICEPS TENDINITIS,DEGENERATIVE CHANGES WITH INTERSTITIAL TEARS NOTED IN PASRT OF SUPRASPINATUS, SUBCORTICAL BURSITIS
USG ABDOMEN_ BULKY LEFT KIDNEY WITH ALTERED ECHOTEXTURE WITH UPPERPOLE CALCULUS
ENDOSCOPY- SMALL HIATUSERNIA
ECG; NORMAL SINUS RHYTHM, SINUS T HACHYCARDIA
HEMOGRAM:
HB-11.5,11.6,11.5
TLC-9300,6600,6200
PLT-2.66'2.04,2.44
COURSE IN HOSPITAL:
TREATMENT GIVEN
I V FLUIDS NS,RL@ 75ML/HR
IMJ.NEOMOL 1GM IV/SOS
INJ.PAN 40MG IV/OD
INJ.ZOFER 4 MG IV/SOS
T.DOLO 650 MG PO/TID
T.PROPONOLOL 40 MG PO/BD
CANDID ORAL PAINT LA TID
ZYTEE GEL AFTER FOOD TID
BETADINE 3% GARGTAB . CARBIMAZOLE 10MG/PO/TID
TAB. PROPONOLOL 20MG PO/TID
TAB TELMA 40MG PO/OD
TAB ULTRACET PO/BD FOR 2 DAYS
TAB OLANZAPINE 5MG PO/HS
TAB.PAN 40MG PO/OD
TAB.TENDOCARE PO/OD
TAB.SHELCAL PO/OD
SYSTAPHLEM GEL FOR L/A
SYP. LACTULOSE 15ML PO/TID
SYP POTKLOR 10 ML/PO/TID WITH GLASS OF WATER
S
AMC Bed 3
14.05.23
50 year old female
A
pyrexia under evaluation
S
drowsy
difficulty in swallowing increased
Fever spikes present
loss of appetite , appetite decreased comparitively
Complaints of knee pain decreased when compared to the day of admission
Stools not passed
O
Patient is c/c/c
Temp:- 99.2
PR- 149bpm
RR - 38cpm
BP- 140/80mmHg
GRBS- 96mg%
CVS- S1s2present, no murmurs heard
RS-B/L air entry present
NVBS present
PA- soft,NT
CNS - NFND
A
Pyrexia under evaluation
P:
1)IV fluids NS, RL @ 75ml/hr
2) Inj. neomol 1g/IV/SOS (If temp >101°F)
3) Inj. Zofer 4mg/PO/SOS
4)Tab. PAN 40mg PO/OD
5)Tab.Dolo 650mg PO/BD
6)Temp monitoring 2nd hrly
7) Vitals monitoring hrly
AMC Bed 3
15.05.23
50 year old female
S
drowsy
cannot sleep yesterday night .
difficulty in swallowing decreased
Fever spikes present with chills
appetite increased comparitively but cannot eat due to bitter tongue
Complaints of knee pain decreased when compared to the day of admission
complaints of shoulder pain , not decreased
Stools not passed
O
Patient is c/c/c
Temp:- 99.8
PR- 131bpm
RR - 38cpm
BP- 180/100mmHg
CVS- S1s2present, no murmurs heard
RS-B/L air entry present
NVBS present
PA- soft,NT
CNS - NFND
A
HYPERTHYROIDISM
P:
1)IV fluids NS, RL @ 75ml/hr
2) Inj. neomol 1g/IV/SOS (If temp >101°F)
3) Inj. Zofer 4mg/PO/SOS
4)Tab. PAN 40mg PO/OD
5)Tab.Dolo 650mg PO/BD
6)Temp monitoring 2nd hrly
7) Vitals monitoring hrly
8)PROPONOLOL 40mg Po/BD
9)TAB .CARBIMAZOLE 10mg PO/TID
10) BETADINE 3% GARGLES
AMC Bed 3
16.05.23
50 year old female
S
drowsy more than yestersay
difficulty in swallowing decreased.
Cannot hold neck.
Fever spikes present
appetite decreased
Complaints of knee pain decreased when compared to the day of admission
complaints of shoulder pain , not decreased
Stools passed.
O
Patient is c/c/c
Temp:- 98.8
PR- 148bpm
RR - 28cpm
BP- 140/80mmHg
GRBS- 70 mg%
CVS- S1s2present, no murmurs heard
RS-B/L air entry present
NVBS present
PA- soft,NT
CNS - NFND
A
HYPERTHYROIDISM
P:
1)IV fluids NS, RL @ 75ml/hr
2) Inj. neomol 1g/IV/SOS (If temp >101°F)
3) Inj. Zofer 4mg/PO/SOS
4)Tab. PAN 40mg PO/OD
5)Tab.Dolo 650mg PO/BD
6)Temp monitoring 2nd hrly
7) Vitals monitoring hrly
8)PROPONOLOL 40mg Po/BD
9)TAB .CARBIMAZOLE 10mg PO
/TID
10) BETADINE 3% GARGLES
AMC Bed 3
17.05.23
50 year old female
S
drowsy
sleep cycle altered
difficulty in swallowing decreased.
Cannot hold neck.
Fever spikes present
appetite decreased , nausea vomiting +
Complaints of knee pain decreased when compared to the day of admission
complaints of shoulder pain , increased
Stools passed.
O
MMSE:
Orientation to time +5
Orientation to place : +5
registration: +1
Attention: 1
Recall:1
Naming:2
Repitition:1
doing and obey: 0
sentence:1
copying:1
MMSE :(18/30)
Patient is c/c/c
Temp:- 98.8
PR- 112bpm
RR - 27cpm
BP- 140/80mmHg
GRBS- 112mg%
CVS- S1s2present, no murmurs heard
RS-B/L air entry present
NVBS present
PA- soft,NT
A
HYPERTHYROIDISM
P:
1)IV fluids NS, RL @ 75ml/hr
2) Inj. neomol 1g/IV/SOS (If temp >101°F)
3) Inj. Zofer 4mg/PO/SOS
4)Tab. PAN 40mg PO/OD
5)Tab.Dolo 650mg PO/BD
6)Temp monitoring 2nd hrly
7) Vitals monitoring hrly
8)PROPONOLOL 40mg Po/BD
9)TAB .CARBIMAZOLE 10mg PO/TID
10) BETADINE 3% GARGLES
AMC Bed 3
18.05.23
50 year old female
S
drowsy
sleep cycle altered
difficulty in swallowing decreased.
Fever spikes present
appetite decreased , nausea vomiting +, non projectile ,non bilious associated with nausea 2 times in last day
Complaints of knee pain decreased when compared to the day of admission
complaints of shoulder pain , increased
Stools passed.
O
MMSE:
Patient is c/c/c
Temp:- 98.8
PR- 128bpm
RR - 27cpm
BP- 150/90mmHg
GRBS- 109mg%
CVS- S1s2present, no murmurs heard
RS-B/L air entry present
NVBS present
PA- soft,NT
A
HYPERTHYROIDISM
P:
1)IV fluids NS, RL @ 75ml/hr
2) Inj. neomol 1g/IV/SOS (If temp >101°F)
3) Inj. Zofer 4mg/PO/SOS
4)Tab. PAN 40mg PO/OD
5)Tab.Dolo 650mg PO/BD
6)Temp monitoring 2nd hrly
7) Vitals monitoring hrly
8)PROPONOLOL 40mg Po/BD
9)TAB .CARBIMAZOLE 30mg PO/TID
10) BETADINE 3% GARGLES
Cubicle Bed 1
21 .05.23
50 year old female
S
drowsy
Fever spikes present
sleep cycle altered
appetite decreased
Complaints of knee pain decreased when compared to the day of admission
complaints of shoulder pain , increased
Stools passed.
O: drowsy ,not cooperative
Patient is c/c/c
Temp:- 99.8
PR- 115bpm
RR - 26cpm
BP- 130/80mmHg
CVS- S1s2present, no murmurs heard
RS-B/L air entry present
NVBS present
PA- soft,NT
A
HYPERTHYROIDISM
P:
1)IV fluids NS, RL @ 75ml/hr
2) Inj. neomol 1g/IV/SOS (If temp >101°F)
3) Inj. Zofer 4mg/PO/SOS
4)Tab. PAN 40mg PO/OD
5)Tab.Dolo 650mg PO/BD
6)Temp monitoring 2nd hrly
7) Vitals monitoring hrly
8)PROPONOLOL 40mg Po/BD
9)TAB .CARBIMAZOLE 10mg PO/TID
10) BETADINE 3% GARGLES
11) Inj KCL 2amp (50mEq) in 500ml NS/IV slowly over 5 hours/STAT.















Comments
Post a Comment